Table of Contents
Do your legs feel tired, heavy and achy? Have you noticed swollen, ropy looking veins that cause your legs to look bumpy? You might have varicose veins. Varicose veins are common and can appear on almost any part of the body, but most commonly occur in the lower limbs.
While they may not be deadly, they can lead to discomfort, pain and other health issues if left untreated. In this post, we’ll explore varicose vein symptoms and treatments, so you can determine what course of action is right for you. In general, varicose veins are no serious health issue. These can be uncomfortable to look at, but can sometimes be harmful with long-term health issues.

Varicose Vein Disease Overview
What are varicose veins?
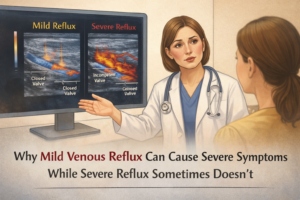
Varicose vein disease is a condition that occurs when veins become damaged and fail to adequately return blood to the heart, leading to high blood pressure. It affects many parts of the body, from superficial veins in the legs and arms to deep veins located in muscles.
What are the symptoms of varicose veins?
Symptoms of venous disease include swelling, pain, itchiness, discoloration of skin, skin ulcers, and increased risk of infection. In more severe cases, clotting can occur inside the vein, which can lead to pulmonary embolism or other serious medical events.
What are the risk factors of varicose veins?
Risk factors for venous disease include advancing age; those who are overweight or obese; sedentary lifestyle; prolonged sitting or standing; pregnancy; smoking; family history; prior trauma to the limb; and medical conditions such as deep vein thrombosis or varicose veins.
How do you diagnose varicose veins?
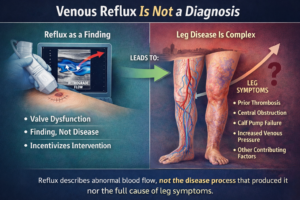
Diagnosis is typically made through physical examination, as well as imaging tests, such as ultrasound, magnetic resonance imaging (MRI), computed tomography (CT) scans.
It is important for those at risk of developing venous disease to take steps to prevent it before symptoms develop, and monitoring for any unusual changes in their limbs that could indicate a problem.
The causes of varicose vein disease
Varicose veins are a common condition that occurs when veins become swollen, enlarged and twisted. This is due to a combination of factors, including genetics and lifestyle, as well as pressure or trauma inflicted on the vein walls.
Generally, aging is responsible for weakened vein walls and valves, which can lead to varicose veins.
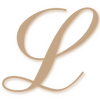
The most common cause of varicose veins is venous reflux, which occurs when the internal one-way valves become damaged and allow blood to flow in the wrong direction. This causes an accumulation of blood around the valve, resulting in increased pressure on vein walls and stretching them outwards.
Over time, this can cause the vein to swell and twist, making it visible beneath the skin’s surface.

Other common causes of varicose veins include pregnancy, obesity, and physical inactivity.
During pregnancy, body weight increases significantly, while hormones such as progesterone make it more difficult for blood to pass through the vessels by relaxing their walls. Being overweight also puts extra strain on veins due to increased pressure placed on them from above.
Finally, physical inactivity can contribute, as lack of movement does not allow muscles to pump enough blood from these areas back up towards the heart, leading to a backup in these vessels, eventually leading to varicose veins.
In conclusion, it is important to understand that there are multiple contributing factors that lead to varicose veins, including age-related weakening of vein walls and valves, as well as lifestyle choices or traumatic events like pregnancy or being physically inactive for extended periods of time. Regular exercises, such as walking or jogging, can help prevent venous reflux associated with varicose veins by promoting healthy circulation of blood throughout your body.
What are the signs and symptoms of varicose veins?
The most common signs of varicose veins are visible, protruding veins that are blue, dark purple, or flesh-coloured. They can be twisted, bulging, and often appear in clusters on the legs, ankles and feet.
Other symptoms of varicose veins include swelling or heaviness in the legs; burning or itching sensations in the area of the veins; aching or cramping in the legs; leg fatigue; skin discoloration around the ankles; and skin ulcers near the ankles.
Varicose veins may also cause pain when standing for long periods of time, as well as a feeling of restlessness in the legs, especially at night.
In addition to these physical symptoms, psychological effects, such as decreased self-esteem, can occur due to embarrassment over visible varicose veins. In severe cases, there is an increased risk of complications, such as blood clots, dermatitis, and deep vein thrombosis (DVT).
How do you know if you have vein problems?
If you suspect that you may have vein problems, there are certain symptoms to look out for. Generally, a feeling of discomfort or pain in the legs is one tell-tale sign. This sensation can range from a mild ache to feeling like your muscles are being stung by something.
Additionally, if you experience swelling in the legs or any areas of heat and burning sensations, this could also be indicative of vein issues.
Another symptom to be aware of is discomfort after sitting or standing for long periods of time. You may find that your legs feel heavy or tired and that it is uncomfortable or even painful to move them afterwards. Itching in a particular vein is also another potential sign that something is wrong and should not be ignored. If this is present, it’s recommended to seek medical attention as soon as possible.
In more severe cases, varicose veins may become visible as thickened and discoloured veins on the surface of the skin. Furthermore, other problems associated with vein issues such as leg ulcers could develop if left untreated. These open sores can cause further pain and itchiness, but can usually be avoided with proper management.
If any of these symptoms persist or worsen over time, it’s best to visit a vein doctor who will be able to properly diagnose you and determine the best course of treatment for your specific case.
Preventing varicose veins
Preventing varicose veins is an important step in controlling the disease. Taking measures to reduce the risk of varicose veins can help to minimise the severity and frequency of your symptoms. Some preventive strategies may include:
Avoiding standing or sitting for long periods of time
Varicose veins can form when you remain in a standing or sitting position for too long, which puts increased pressure on the veins. If you must remain standing for a significant period of time, make sure to take frequent breaks and shift positions when able.
Exercising regularly
Regular physical activity helps increase circulation and reduce pressure on the veins. Aim to move throughout the day and dedicate some time each day to exercising, like taking a walk or participating in yoga, aerobics, or swimming.
Maintaining a healthy weight
Being overweight places additional strain on the veins and can contribute to varicose vein formation; losing excess weight may help relieve some of that strain. Eating a balanced diet full of fruits and vegetables can also promote healthy weight management.
Wearing compression stockings or special support hose.
Wearing these items can help reduce swelling in your legs by increasing circulation while minimising pressure on your veins; they are especially useful if you spend most of your day sitting or standing in one place (like at work).
Elevating your legs
Putting your legs up above heart level when possible may reduce pain associated with varicose veins by providing relief from gravity’s pull downwards. Finally, avoid wearing tight clothing as this can cause constriction that further reduces circulation to the area affected by varicose veins.
What are the treatments for varicose veins?
Varicose veins treatment typically includes a combination of lifestyle modifications, compression therapy, medications, and sometimes surgery. It is important for patients to discuss all treatment options with their vein doctor before beginning any varicose vein treatment program, in order to ensure that they get the best care possible for their specific condition.
Lifestyle modifications
Making lifestyle changes is an important part of maintaining good health and wellness. There are many different ways that people can adjust their habits to benefit both their physical and mental wellbeing. Eating a healthy, balanced diet is one of the most fundamental elements of this process, as it provides the body with the nutrients it needs to thrive.
Exercising regularly is another key factor when it comes to making lifestyle changes for improved health. Finding activities that you enjoy can be extremely beneficial in terms of staying motivated to exercise on a regular basis.
Making sure to stay socially connected can have a positive impact on overall wellbeing as well. Keeping up with regular check-ins with friends and family members can help us feel more supported during difficult times.
Ultimately, making lifestyle changes takes time and dedication, but the results are well worth the effort! By taking proactive steps towards healthier habits, we’ll not only feel better physically, but also experience emotional benefits; having an overall sense of wellbeing that we can carry throughout our lives no matter what comes our way.

Compression therapy
involves wearing special stockings or socks to help manage swelling in the legs and feet. The compression should be tight enough to provide the desired amount of pressure on your lower limbs, but not so tight that it leaves you uncomfortable and in pain. It’s important to choose a well-fitting stocking that isn’t too restrictive and gives you maximum comfort.
Surgery
is typically considered when other treatments are not effective.
Modern procedures
Procedures such as sclerotherapy, ligation & stripping, and endovenous laser ablation can be used to close veins that cannot be treated with lifestyle changes or compression therapy alone.
It’s important to note that while most people see results immediately following their treatment, full healing can take anywhere from two weeks up to six months, depending on individual cases.
Overall, endovenous laser treatment is an effective way to treat varicose veins without having to undergo more invasive alternatives, such as surgery or sclerotherapy. It has become increasingly popular among patients, especially since it does not require hospitalisation or general anaesthesia and its high success rate means patients can expect their veins to stay closed over time with minimal complications in most cases.
Can vein disease be cured?
Unfortunately, vein disease cannot be cured. Venous insufficient systemic vascular disorder is a disorder that causes poor circulation in the veins of the legs, resulting in swelling and pain.
The condition is thought to occur when veins become damaged or weakened over time, and can cause serious complications if left untreated. In some cases, symptoms may improve with lifestyle changes, such as exercise and weight loss. However, there is no cure for venous insufficiency, so people affected by the condition must focus on managing their symptoms in order to reduce their risk of further damage.
Resources:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/varicose-veins
https://www.healthdirect.gov.au/varicose-veins
https://www.mayoclinic.org/diseases-conditions/varicose-veins/symptoms-causes/syc-20350643