A blow-out or burst vein can rupture due to a needle insertion when drawing blood for a blood test. The term “Blow veins” or ruptured vein, though it sounds serious, can be quite dangerous for most people.
This article delves into the potential dangers of vein rupture, exploring the various factors that can lead to this condition, its symptoms, and the importance of prompt medical attention. Discover the implications and preventive measures for maintaining vascular health.
Can Varicose Veins Burst?

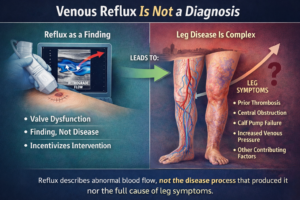
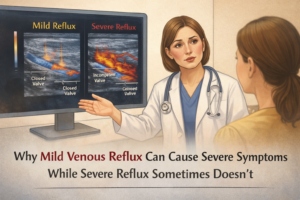
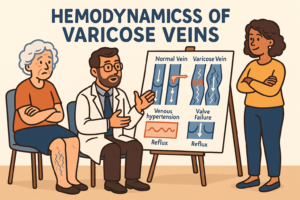
Varicose veins are enlarged and twisted veins in the legs. Varicose veins burst due to weakened vein walls and increased pressure. Factors like trauma, injury, and chronic venous insufficiency increase the risk of ruptured vein. Trauma, straining, heavy lifting, and prolonged standing can also cause rupture. Chronic venous insufficiency weakens veins, increasing the risk of varicose vein ruptures, skin changes and leg ulcer. Most cases do not result in ruptured varicose veins or blown veins, but in the case of a ruptured varicose vein or blown vein, bleeding can range from minor to significant.
What Happens if You Pop a Vein?
Popping a vein is the rupture or damage of a blood vessel, often caused by trauma or injury. It most commonly happens at the injection site of a needle insertion when drawing blood on when a healthcare professional attempts a line insertion.The consequences of a popped vein include bleeding, haematomas, infection, and blood clotting.
Bleeding can range from minor to significant, and the severity of the injury determines the need for medical attention. Hematomas cause swelling, pain, and discoloration, while infection can lead to inflammation, redness, and fever.
Blood clotting may also occur to stop bleeding, but it can increase the risk of complications like deep vein thrombosis.
Seeking medical attention is crucial, as healthcare professionals can assess the injury’s severity, provide treatment, and determine if further intervention is necessary.
What Are the Symptoms of a Burst Varicose Vein?

When a varicose vein bursts, it can cause various symptoms. Common symptoms include minor to significant bleeding, pain, swelling, bruising, tender or warm skin, and clot formation.
To address a ruptured varicose vein or blown vein, seek medical attention immediately, apply pressure, elevate the leg, and cover the affected area with a clean cloth or bandage.
A medical evaluation is necessary to assess the rupture’s extent, control bleeding, and provide appropriate treatment.This is especially important if you are on blood thinners.
Healthcare professionals may recommend wound care, compression bandaging, or surgical intervention to address the burst varicose vein and prevent further complications.
Risk Factors for Varicose Vein Bursting
Varicose veins can burst due to various factors, including severity, trauma, age, gender, pregnancy, obesity, prolonged standing or sitting, and family history.
Severe varicose veins increase the risk of bursting, while trauma or injury can trigger rupture. Age also increases the risk, especially in individuals over 50.
Women are more likely to develop varicose veins, and hormonal changes during pregnancy and menopause can contribute to vein bursting. Pregnancy also puts pressure on veins, while obesity increases the risk of varicose vein complications.
Prolonged standing or sitting can hinder blood circulation and contribute to vein development. Family history may also increase the risk of varicose vein bursting.
Can you get a blood clot from a burst varicose vein?

A burst varicose vein rupture does not lead to the formation of a blood clot, known as a thrombus. However, a varicose vein can.
The risk of developing a blood clot is influenced by factors such as the varicose vein size and severity, extent of the venous disease, and individual predisposing factors such as long flight and immobility.
Deep varicose vein thrombosis (DVT) causes pain, swelling, warmth, and redness in the affected leg.
Risk factors include blood clotting disorders, prolonged immobility, obesity, smoking, or a family history of blood clots.
How Can I Prevent a Varicose Vein from Bursting?
To reduce the risk of varicose vein bursting, maintain a healthy weight, stay active, avoid prolonged sitting or standing, elevate legs, wear compression stockings, avoid tight clothing, take breaks during pregnancy, and treat underlying venous conditions.
These measures can help improve blood circulation and strengthen vein-supporting muscles.
However, not all varicose veins can be completely prevented or eliminated. Consult a healthcare or medical professional first for accurate diagnosis, personalised advice, and appropriate treatment options
Treating Popped Varicose Veins and Blood Vessels

Popped varicose veins or burst blood vessels require medical attention for evaluation and medical treatment.
Common approaches include direct pressure and elevation, wound care, compression bandaging, surgical interventions, and follow-up care.
Direct pressure and elevation can control minor bleeding, while wound care involves cleaning and applying sterile dressings.
Surgical interventions, such as ligation or removal, may be necessary for severe or recurrent ruptures or complications.
Follow-up care is essential to monitor healing, assess complications, and provide further guidance.
How to Apply Pressure To The Popped Vein
Applying direct pressure to a popped vein to control bleeding is crucial.
First, clean your hands, locate the bleeding site, use a clean cloth or gauze pad, and maintain pressure for 10-15 minutes.
If bleeding persists, apply additional layers of cloth or gauze, and seek medical attention urgently especially if profuse or unstoppable excessive blood loss.
Elevate the affected limb if possible to reduce blood flow to surrounding tissue and control bleeding. It’s important to seek medical attention promptly to evaluate the severity of the situation and receive appropriate treatment.
How To Treat Varicose Veins Before They Burst?
Varicose vein treatment options depend on the severity of the condition and symptoms experienced.
Common approaches include lifestyle changes, compression therapy, sclerotherapy, endovenous ablation, vein stripping and ligation, ambulatory phlebectomy, and laser or radiofrequency ablation.
Lifestyle changes, exercise, and avoiding prolonged periods of sitting or standing can alleviate symptoms and prevent worsening.
Compression therapy, sclerotherapy, and endovenous ablation are minimally invasive procedures that help the veins collapse and be reabsorbed.
Surgical procedures like vein stripping and ligation may be recommended for severe cases or when other treatments have not been successful.