Did you know that 1 in 3 Australians can develop varicose veins? This condition affects millions, making it key to know the signs and how to manage it. Varicose veins are more than just a beauty issue; a varicose vein can cause serious health problems if ignored.
Varicose veins are a symptom of chronic venous insufficiency, a condition where the veins have trouble sending blood from the legs back to the heart.
It is important to get varicose veins diagnosed by a healthcare professional, who may use a duplex ultrasound to check blood flow and the structure of the leg veins.
Key Takeaways
Varicose veins are a common condition affecting 1 in 3 Australians
Understanding the symptoms is the first step in managing varicose veins
Risk factors include age, pregnancy, obesity, and a sedentary lifestyle
Lifestyle changes like regular physical activity can help prevent and manage varicose veins
Seeking early treatment can alleviate symptoms and prevent complications
We’ll look into the common signs of varicose veins, the causes, and ways to stop and handle this issue. This guide aims to help you understand your vein health better, whether it’s for you or someone you care about.
What are Varicose Veins?
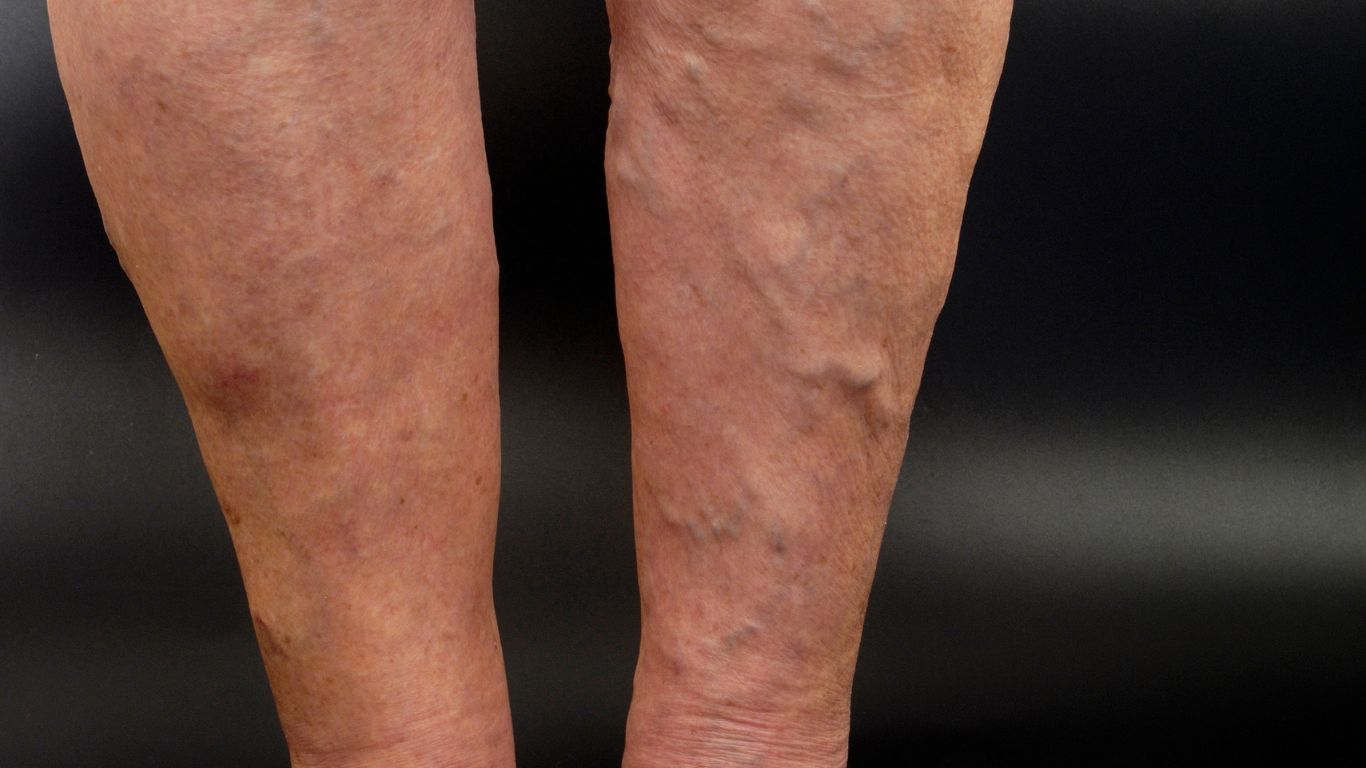
Varicose veins make the veins in your legs swell and twist, showing under the skin as swollen blood vessels. Varicose veins occur when the veins get weak and their valves don’t work right. This lets blood pool and the veins bulge. As a result, those weak or damaged valves lead to varicose veins . As more blood pools in the damaged vein, small varicose veins become larger varicose veins
Understanding Vein Walls and Blood Flow
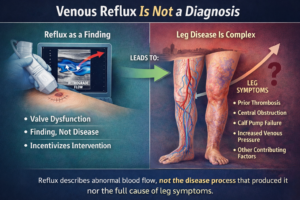
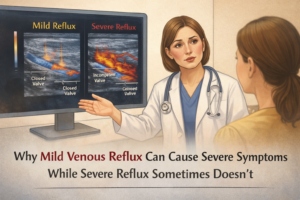
Veins carry blood that’s low on oxygen back to the heart. They have strong walls and one way valves to keep blood moving the right way. But with varicose veins, the walls get weak and one way valves break, causing blood to flow back and pool, a condition known as venous reflux.
Risk Factors for Varicose Veins
Some things can make you more likely to get varicose veins, like:
Family history – It often runs in families, showing it might be genetic.
Age – Getting older, especially after 50, raises the risk.
Gender – Women get them more often than men, thanks to hormones, hormonal changes, and pregnancy.
Obesity – Being overweight adds pressure on your leg veins.
Pregnancy – Pregnancy’s extra weight and pressure make veins stand out more.
Sedentary lifestyle – Not moving much or prolonged standing can slow blood flow and cause varicose veins.
Knowing what causes and increases the risk of varicose veins helps in managing it. In severe varicose veins, complications such as long-term swelling, nonhealing sores, and blood clots can occur, necessitating prompt medical attention to treat varicose veins.
What is the difference between varicose veins and spider veins?
Varicose veins and spider veins are both common venous conditions, but they differ significantly in appearance, symptoms, and severity. Varicose veins are larger, swollen veins that are often raised and appear twisted, typically in shades of blue or purple. They are most commonly found on the legs and can cause symptoms like aching, heaviness, swelling, and discomfort. In contrast, spider veins are much smaller, appearing as thin, web-like patterns close to the skin’s surface, and are usually red, blue, or purple. Spider veins are often found on the legs and face and are primarily a cosmetic concern, though they can occasionally cause mild discomfort. While varicose veins are caused by more significant vein valve issues, leading to blood pooling and vein enlargement, spider veins are typically caused by similar but less severe factors, such as sun exposure, hormonal changes, or minor vein damage. Treatment for varicose veins may involve lifestyle changes or medical procedures, while spider veins are usually treated for cosmetic reasons with less invasive options like sclerotherapy or laser therapy.
Common Symptoms of Varicose Veins
Varicose veins are a common issue in Australia. They can cause various symptoms. It’s important to know these symptoms to get help early and manage a varicose vein condition well.
One main symptom is twisted, bulging veins under the skin. These veins can be blue, purple, or red. They are often seen on the legs, thighs, or near the pelvis. People with varicose veins might feel their legs are heavy, aching, or throbbing, especially after sitting or standing a lot. Some people may also experience leg cramps, swollen ankles and restless legs, especially at night.
Varicose veins can also change the skin’s look and feel. Some may see their skin turn reddish or brownish. It might look scaly or itchy. In worse cases, the skin could get hard or even open up sores, needing quick doctor’s care.
In severe cases, varicose veins can lead to the formation of blood clots, which require urgent medical care.
Not everyone with varicose veins will have all these symptoms. How bad and what symptoms you get can differ. It’s key to see a doctor if you notice any vein-related changes or worries.
Symptom Description Visible Bulging Veins Twisted, swollen veins that are visible under the skin, often blue, purple, or red in colour. Aching or Throbbing Sensations A feeling of heaviness, aching, or throbbing in the affected areas, particularly after prolonged standing or sitting. Skin Changes Reddish or brownish discoloration, as well as a scaly or itchy appearance on the skin. Hardened or Ulcerated Skin In more severe cases, the skin can become hardened or develop ulcers, requiring prompt medical attention.
If you’re showing any of these varicose vein symptoms, seeing a healthcare professional is a must. They can give you the right diagnosis and treatment plan.
Prevent Varicose Veins: Lifestyle Changes
Keeping active and doing regular exercises is key to stopping varicose veins. These activities help improve blood flow and ease the strain on your veins. This can reduce the risk of these conditions.
Elevating legs and maintaining a healthy weight are also important in preventing varicose veins.
Physical Activities and Compression Stockings for Better Circulation
Adding these exercises to your daily life can boost blood flow and stop varicose veins:
Regular walking: Take brisk walks for at least 30 minutes each day to get your blood moving.
Swimming: Swimming is great for circulation without putting too much pressure on your legs.
Leg raises: Do simple leg-raising exercises while sitting or lying down to help blood flow better.
Calf raises: Doing calf raises strengthens your lower leg muscles and helps with blood return.
It’s also important to not sit or stand for too long. Make sure to take breaks and elevate your legs. This helps prevent varicose veins.
Physical Activity Benefits for Varicose Vein Prevention Walking Improves blood flow and strengthens leg muscles Swimming Low-impact exercise that promotes circulation without added pressure on legs Leg Raises Helps improve venous return and reduce pooling of blood in the legs Calf Raises Strengthens the muscles in the lower legs, aiding in venous return
By making these lifestyle changes and staying active, you can stop varicose veins before they start. This keeps your legs healthy and looking good.
Family History and Varicose Veins
If you have family members with varicose veins, you might be more likely to get them too. Genetics and hereditary factors can greatly affect the formation of these veins. They can be unsightly and sometimes painful.
A genetic predisposition can significantly increase the likelihood of developing varicose veins.
Studies show that if a close relative, like a parent or sibling, has varicose veins, you’re more at risk. This risk comes from the shared genes passed down through families.
Having both parents with varicose veins increases your risk even more. This means certain genetic traits or a mix of factors can make it more likely for you to get them.
Having a family history of varicose veins doesn’t mean you’ll definitely get them. But knowing the risk is important. It helps you take steps to manage and maybe prevent them.
Family History Increased Risk of Varicose Veins One parent with varicose veins 2-3 times higher Both parents with varicose veins 4-5 times higher
Regular health check-ups, a healthy lifestyle, and watching for early signs can help manage varicose veins. Even with a family history.
Complications of Varicose Veins and Spider veins
Varicose veins and spider veins, while often viewed as cosmetic concerns, can lead to various complications if left untreated. Severe Varicose veins are more likely to cause significant health issues, such as chronic pain, swelling, blood clots and a heavy sensation in the legs.
Over time, they can lead to more severe conditions like skin changes, including discoloration and thickening, or the development of venous ulcers, which are slow-healing sores. Additionally, varicose veins can increase the risk of blood clots, including deep vein thrombosis (DVT), a potentially life-threatening condition.
Spider veins, on the other hand, typically pose fewer health risks and are mostly a cosmetic issue. However, in some cases, they can cause mild discomfort, such as itching or burning, and may indicate underlying venous insufficiency that could progress to more serious complications if not addressed.
Both conditions can significantly affect the quality of life, emphasising the importance of timely evaluation to treat varicose veins.
Recognizing Early Signs and Symptoms
It’s key to spot the early signs of varicose veins to act fast and stop it from getting worse. Knowing the changes in your leg veins lets you get medical help early. This can prevent the condition from getting more serious.
Recognizing Early Signs and Symptoms
One of the first signs of a varicose vein is seeing small, twisted veins under the skin. These veins can look blue, purple, or red. They often show up on the legs, especially around the ankles and calves.
Visible, twisted or bulging veins in the legs
Aching, heavy, or tired legs, especially after standing or sitting for long periods
Swelling in the legs or ankles, particularly towards the end of the day
Itching or irritated skin around the affected veins
Changes in skin color, such as reddish or brownish discoloration, around the affected veins
If you see any of these early signs of varicose veins, get medical help. A doctor can check your condition, diagnose varicose veins and suggest the best options to get your varicose veins treated. This can help manage the symptoms of varicose veins and stop them from getting worse.
“Paying attention to the early signs of varicose veins and addressing them promptly can make a significant difference in managing the condition and preventing it from progressing.”
Treatment Options for Varicose Veins
If you’re facing the discomfort and unsightly look of a varicose vein, there are many options for treating varicose veins.
Compression therapy is a key treatment for varicose veins. It involves wearing special stockings or socks that create gentle pressure. This improves blood flow, helps to relieve symptoms and reduces the look of varicose veins and spider veins. For some, this might be enough treatment. Healthcare providers recommend that patients continue to wear compression stockings to manage symptoms associated with long-term vein issues. While varicose veins typically affect superficial veins, it is important to be aware of the risk of deep vein thrombosis, a serious condition involving blood clots in the deeper veins.
For more serious cases, your doctor might suggest minimally invasive procedures. Options include endovenous laser treatment or sclerotherapy to remove varicose veins. These methods aim to collapse or inject veins, making them disappear. These treatments to remove varicose veins are effective to relieve symptoms and have a quick recovery time compared to surgery. Proper diagnosis of varicose veins, often involving a duplex ultrasound, is crucial for determining the most effective treatment plan.
FAQ
What are the common symptoms of varicose veins?
Visible bulging or swollen veins, aching or throbbing sensations in the legs, and a heavy or tired feeling in the legs are common symptoms, along with skin discoloration. You might also notice skin changes like itching.
What are the risk factors for developing varicose veins?
Risk factors include family history, age, pregnancy, obesity, and jobs that involve a lot of sitting or standing. Being overweight and not staying active can also increase your risk.
How can I prevent varicose veins?
To prevent varicose veins, keep a healthy weight and stay active. Elevate your legs when you can, and avoid sitting or standing for too long. Regular exercise helps improve circulation too.
How is family history linked to varicose veins?
Having a family member with varicose veins increases your risk. Genetics and hereditary factors are key in determining your likelihood of getting varicose veins.
What are the early signs and symptoms of varicose veins?
Early signs include small, spider-like veins, slight swelling or discoloration, and a feeling of heaviness or aching in the legs. If you notice these changes, it’s important to seek medical advice.
What are my options when varicose veins develop?
Treatment options range from conservative methods like compression stockings to more advanced procedures. These include sclerotherapy, endovenous laser ablation, or surgery. The best treatment depends on how severe your varicose vein condition is and your individual needs.