Post-thrombotic syndrome is a common and often overlooked complication that can arise after a deep venous thrombosis (DVT). It is characterised by a range of persistent symptoms and complications that can significantly impact a person’s quality of life. In this article, we will explore the causes, risk factors, clinical manifestations, and management options for post-thrombotic syndrome. By increasing awareness and understanding of this condition, we aim to empower individuals affected by PTS and provide valuable insights for healthcare professionals involved in its diagnosis and treatment.
What is Post-Thrombotic Syndrome?

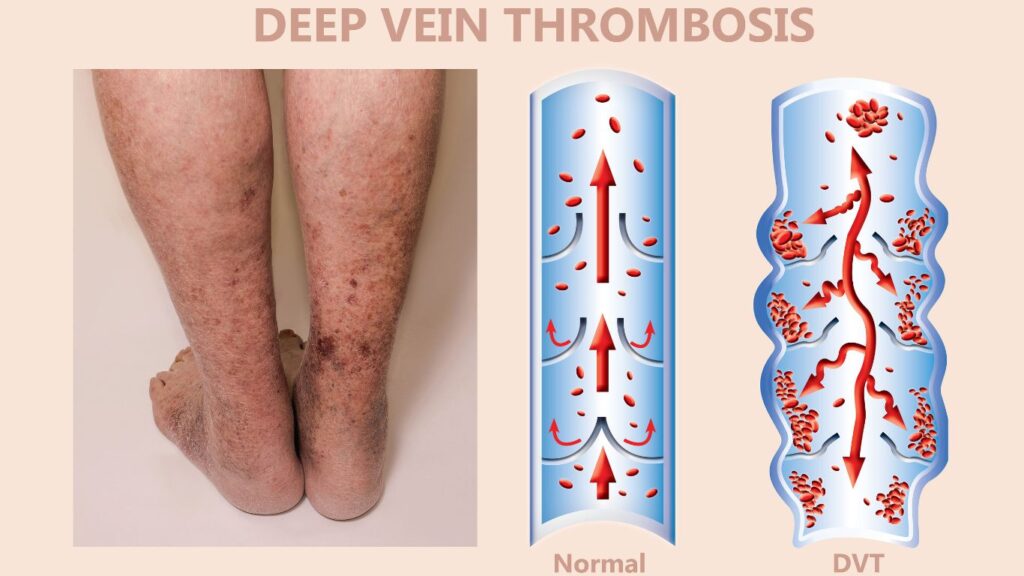
Post-thrombotic syndrome (PTS) is a condition that can occur as a complication of deep vein thrombosis (DVT), a blood clot that forms in a deep vein, usually in the leg. PTS develops when the damaged veins and impaired blood flow resulting from the initial acute deep venous thrombosis. This leads to persistent symptoms and complications even after the clot has been treated or resolved. It is estimated that around 20-50% of individuals who experience deep venous thrombosis will develop post-thrombotic syndrome.
The Difference between Post Thrombotic Syndrome and a Blood Clot (DVT)
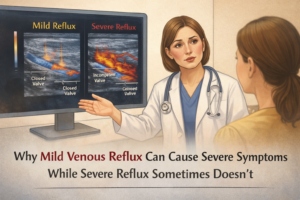
The main characteristic of post-thrombotic syndrome is the presence of long periods of chronic pain and swelling in the affected leg. This creates a form of venous stress disorder. Other common symptoms include heaviness or aching in the leg, cramping, itching, and skin discoloration. In some cases, more severe complications of blood disorders can arise, such as the development of venous leg ulcers, where open sores form on the skin due to poor circulation and tissue damage.
The exact mechanisms of this venous stress disorder behind the development of post-thrombotic syndrome are not fully understood. It is believed to involve a combination of factors including persistent or chronic venous insufficiency, inflammation, and ongoing damage to the vein walls. Certain risk factors may increase the likelihood of developing PTS, such as the extent and location of the initial DVT, repeated episodes of DVT, obesity, older age, and inadequate treatment or management of the initial clot.
What are The Signs of Post-Thrombotic Syndrome?
Post thrombotic syndrome (PTS) can present with a range of signs and symptoms, which can vary in severity and duration. The following are common signs and leg symptoms that may indicate the presence of post-thrombotic syndrome:
1. Chronic leg pain:
Persistent pain in the affected leg, which can be dull, aching, or cramping in nature. The pain may worsen with prolonged standing or sitting.
2. Swelling:
Swelling (oedema) in the affected arm swelling leg, which can range from mild to severe leg heaviness. The swelling may be persistent and may worsen the leg heaviness as the day progresses.
3. Skin changes:
The skin on the affected arm swelling leg may undergo various changes, including thickening, hardening, and discoloration. It may appear red, brown, or bluish in colour. The skin may also feel tight, itchy, or tender.
4. Varicose veins:
The development or worsening of varicose veins, which are swollen and twisted veins that are visible beneath the skin’s surface. Varicose veins may contribute to the discomfort and cosmetic changes associated with post-thrombotic syndrome.
5. Ulcers:
In some cases, severe post-thrombotic syndrome can lead to the development of leg ulcers. These are open sores that typically form around the ankle or lower leg due to poor circulation and tissue damage.
It is important to note that not all individuals who have had a deep venous thrombosis (DVT) will develop post-thrombotic syndrome, and the severity of symptoms can vary from person to person. If you have a history of DVT and experience any of the above signs, it is essential to consult with a healthcare professional for a thorough evaluation and appropriate management.
What is The Underlying Pathophysiology of Post Thrombotic Syndrome?
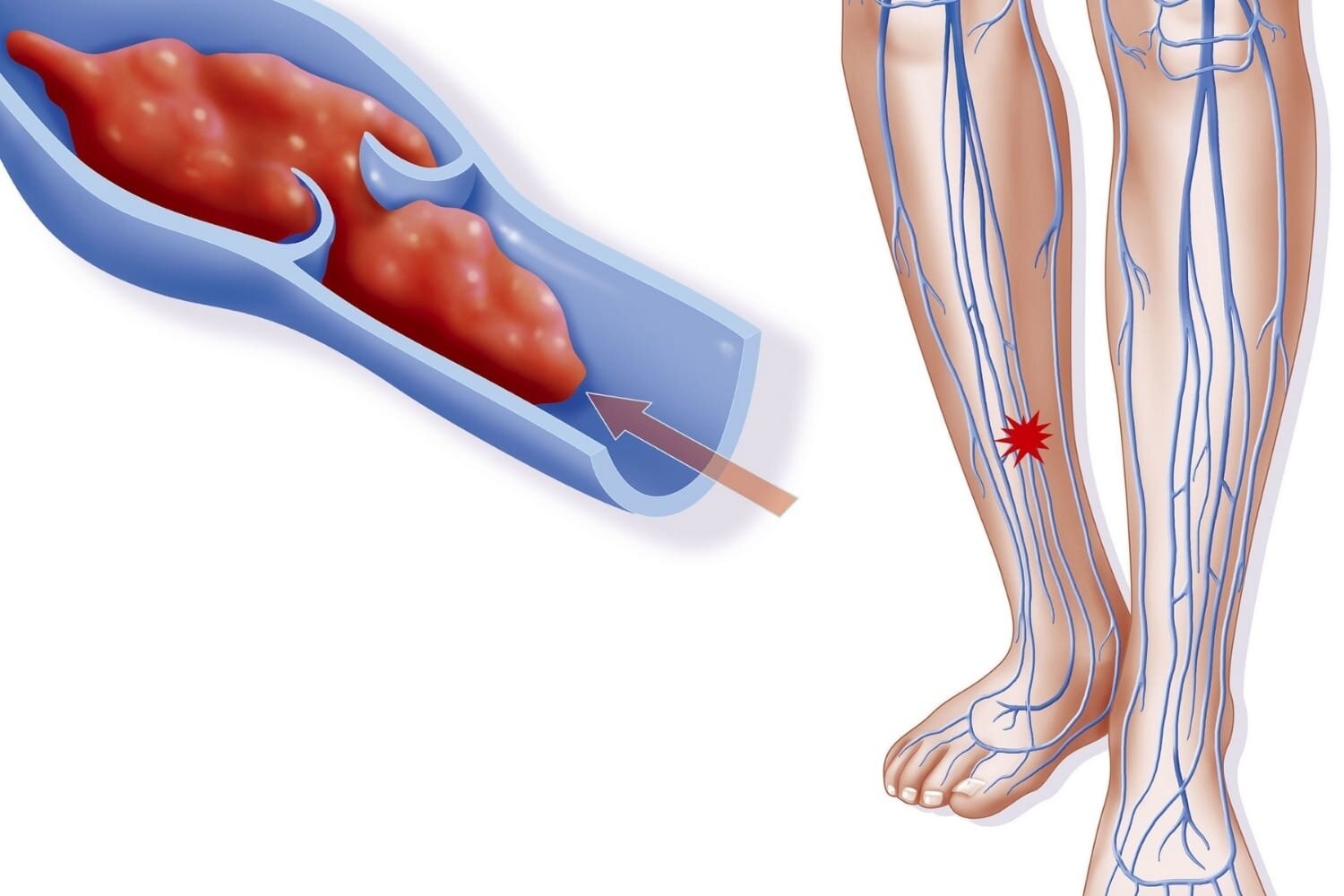
The underlying pathophysiology of post-thrombotic syndrome (PTS) is closely related to the occurrence of deep vein thrombosis (DVT).
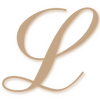
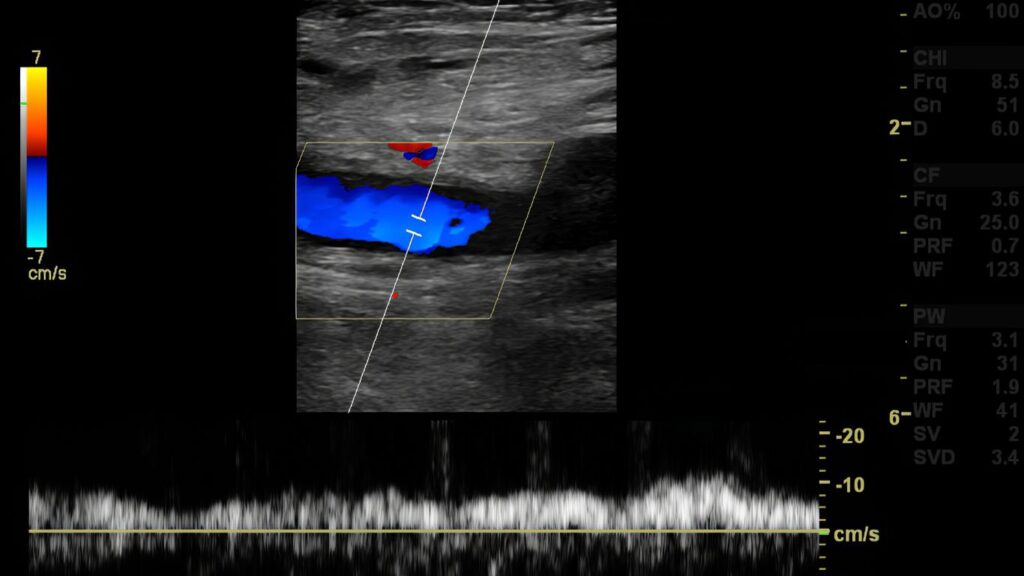
When a venous thrombosis forms in the deep veins of the leg, it can cause obstruction or damage to the normal flow of blood. This leads to increased pressure within the affected leg veins, and impaired circulation.
The obstruction and impaired circulation in the deep veins result in several changes that contribute to the development of PTS. These include:
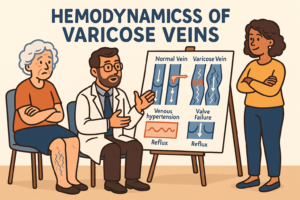
1. Venous valve dysfunction:
The venous valves within the veins, which normally help the blood flows prevent the backflow of blood, may become damaged completely blocked or insufficient due to the DVT. This leads to the reflux of blood and pooling of blood in the lower extremities.
2. Inflammation and tissue damage:
The presence of a DVT triggers an inflammatory response, which can cause injury to the blood vessel walls and surrounding tissues. This inflammation and tissue damage contribute to the development of fibrosis (scar tissue) and remodeling of the affected veins.
3. Impaired lymphatic drainage:
The obstruction of deep veins can also affect the lymphatic system, which is responsible for fluid balance in the body. The impaired lymphatic drainage further exacerbates swelling (edema) and fluid retention in the affected limb.
4. Microcirculatory dysfunction:
The changes in the larger veins can also impact the microcirculation, which includes the smallest blood vessels (capillaries) and the exchange of oxygen, nutrients, and waste products. The microcirculatory dysfunction contributes to tissue hypoxia (lack of oxygen) and further damage to the tissues.
These underlying pathophysiological changes in the venous system, inflammation, tissue damage, lymphatic system, and microcirculation collectively lead to the severe symptoms and complications associated with post-thrombotic syndrome.
It is worth noting that the pathophysiology of PTS is complex and can involve various other factors, including genetic predisposition, recurrent DVTs, and ongoing risk factors. The exact mechanisms may vary from person to person and can influence the severity and progression of the condition.
Incidence and risk factors for Post Thrombotic Syndrome after DVT
The incidence of post-thrombotic syndrome (PTS) after acute deep vein thrombosis, (DVT) varies depending on several factors, including the extent and location of the initial DVT, the adequacy of anticoagulation treatment, and individual patient characteristics. However, it is estimated that approximately 20-50% of individuals who experience a DVT will develop PTS to some degree.
Several risk factors increase the likelihood of developing PTS after a DVT. These include:
1. Extensive DVT:
The presence of a larger blood clot or a prevent blood clots that extend through a significant portion of the deep veins increases the risk of developing PTS.
2. Recurrent DVT:
Individuals who have experienced multiple episodes of DVT have a higher risk of developing PTS compared to those with a single episode.
3. Inadequate anticoagulation:
If anticoagulation therapy is not administered properly or discontinued prematurely, it can increase the risk of recurrent venous thromboembolism and subsequent development of PTS.
4. Obesity:
Being overweight or obese can place additional stress on the veins and impair blood flow, increasing the risk of developing PTS.
5. Older age:
Advanced age is associated with a higher risk of developing PTS, possibly due to age-related changes in vein elasticity and decreased tissue healing ability.
6. Female gender:
Women are more likely to develop PTS than men, potentially due to hormonal factors and differences in vein structure and function.
7. Genetic factors:
Certain genetic conditions, such as deficiencies in natural anticoagulant proteins or mutations that increase the risk of clotting, can predispose individuals to DVT and subsequent PTS.
8. Smoking:
Smoking has been identified as a risk factor for DVT and can also contribute to the development and progression of PTS.
It is important to note that while these factors increase the risk of developing PTS after DVT, not everyone with these risk factors will necessarily develop the condition. Additionally, there may be other individual and environmental factors that influence the likelihood of developing PTS. Close monitoring and appropriate management of DVT, along with lifestyle modifications and adherence to recommended therapies, can help reduce the risk of PTS in individuals with these risk factors.
What is the underlying pathophysiology of PTS?
The underlying pathophysiology of post-thrombotic syndrome (PTS) is closely related to the damage and obstruction caused by a deep vein thrombosis (DVT). When a blood clot forms in a very proximal deep vein thrombosis, it can lead to several changes in the affected vein and surrounding tissues.
1.Acute Deep Venous Thrombosis
During a DVT, inflammation and clotting factors cause the formation of a blood clot within a deep vein, most commonly in the leg. The clot obstructs the normal blood flow through the vein, leading to increased venous pressure and impaired circulation.
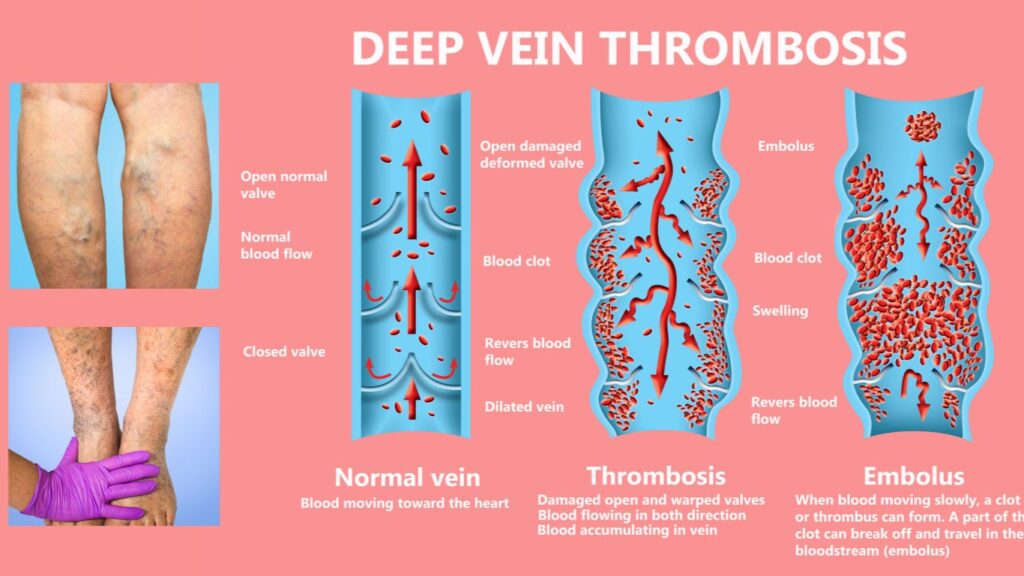
2.Fibrosis
Over time, the clot may partially dissolve, leaving behind residual scar tissue and fibrosis. This fibrotic tissue can cause narrowing and blockage of the affected vein, further impeding blood flow. Additionally, the damaged valves within the vein may no longer function properly, leading blood clots due to reflux or backward flow of blood.
3.Venous Hypertension
The impaired blood flow and increased pressure within the affected vein and surrounding tissues result in various pathological changes. These include chronic venous hypertension, venous dilation (varicosities), and increased capillary permeability. The persistent and chronic venous disease and hypertension can lead to chronic inflammation, tissue damage, and the development of venous leg ulcers in severe cases.
The underlying pathophysiology of PTS is characterized by a combination of venous obstruction, reflux, inflammation, and tissue remodeling. These changes contribute to the chronic symptoms and complications associated with PTS, such as chronic leg pain, swelling, skin changes, and ulcers.
It’s important to note that not all individuals who experience a DVT will develop PTS. The risk of developing PTS varies depending on factors such as the location and extent of the initial clot, the effectiveness of treatment, and individual patient characteristics.
Preventing Post-Thrombotic Syndrome
Preventing post-thrombotic syndrome (PTS) involves early and effective management of deep vein thrombosis (DVT) and minimizing the risk of recurrent blood clots thereafter. Here are some strategies to help prevent the development or progression of PTS:
1. Prompt and proper treatment of DVT:
The timely initiation of anticoagulant therapy for DVT helps prevent clot extension and reduces the risk of complications, including PTS. Adhering to the prescribed treatment plan and attending follow-up appointments are essential.
2. Compression therapy:
Wearing compression stockings or bandages helps improve blood flow and prevents blood pooling in the affected veins. Compression therapy can help reduce swelling, alleviate symptoms, and potentially decrease the risk of developing PTS.
3. Leg elevation:
Elevating the legs above heart level whenever possible can help improve circulation and reduce swelling. Regularly raising the legs for short periods throughout the day can be beneficial.
4. Exercise and physical activity:
Engaging in regular physical activity, as recommended by a healthcare professional, promotes blood flow, strengthens the calf muscles, and helps prevent blood pooling. Low-impact exercises such as walking, swimming, and cycling are often recommended.
5. Weight management:
Maintaining a healthy weight reduces the strain on the veins and improves overall circulation. If overweight or obese, losing weight through a balanced diet and regular exercise can be beneficial in preventing PTS.
6. Avoiding prolonged sitting or standing:
Prolonged periods of sitting or standing can hinder blood flow and increase the risk of blood pooling and clot formation. Taking breaks, stretching, and engaging in leg exercises can help improve circulation.
7. Smoking cessation:
Smoking has been associated with an increased risk of DVT and can worsen vein health. Quitting smoking can improve overall vascular health and reduce the risk of developing PTS.
8. Compliance with medications:
It is important to follow the prescribed medication regimen, including taking anticoagulants as directed and attending follow-up appointments. This helps ensure optimal management of DVT and reduces the risk of complications.
9. Genetic testing and counseling:
In some cases, individuals may have an underlying genetic predisposition to clotting disorders. Genetic testing and counseling can help identify such conditions and guide appropriate preventive measures.
It is crucial to work closely with a healthcare professional experienced in managing DVT and PTS to develop an individualized prevention plan based on your specific needs and risk factors. Early intervention and proactive management can significantly reduce the risk of developing PTS and improve overall outcomes.
How do you treat Post-thrombotic syndrome?
The treatment of post-thrombotic syndrome (PTS) aims to alleviate symptoms, improve quality of life, and prevent further complications. The management to treat post thrombotic syndrome involves a multimodal approach that combines conservative measures and, in some cases, more invasive interventions. Here are some commonly used treatment strategies and options for PTS:
1. Compression Therapy:
Compression therapy is a cornerstone of PTS treatment. It involves wearing compression stockings or bandages that apply graduated pressure on the legs, promoting better blood flow and reducing swelling. Compression helps to alleviate symptoms and prevent progression of the condition.
2. Exercise and Physical Therapy:
Regular exercise and physical therapy can be beneficial in managing PTS. Physical activity promotes circulation, strengthens the leg muscles, and helps reduce symptoms such as pain and swelling. Specific exercises and rehabilitation programs may be prescribed to improve mobility, enhance muscle pump function, and reduce the risk of complications.
3. Medications:
In some cases, medications may be used to manage symptoms associated with PTS. These may include pain relievers to alleviate discomfort, anti-inflammatory drugs to reduce inflammation, or medications to improve blood flow and reduce the risk of blood clots.
4. Intermittent Pneumatic Compression (IPC):
IPC devices are inflatable sleeves, elastic compression stockings, or boots that are periodically inflated and deflated to promote blood flow in the legs. IPC can be used as an adjunct to compression therapy and may help in reducing leg swelling, and improving symptoms.
5. Endovascular Interventions:
In more severe cases of PTS, endovascular interventions may be considered. These minimally invasive procedures aim to improve venous flow by removing or bypassing the obstructed or damaged veins. Techniques such as venous stenting, balloon angioplasty, or venous bypass may be used in selected cases.
6. Lifestyle Modifications:
Adopting a healthy lifestyle can have a positive impact on managing PTS. This may include maintaining a healthy weight, avoiding prolonged sitting or standing, elevating the legs when resting, and practicing good skin hygiene to reduce the risk of complications like venous ulcers.
The treatment plan for PTS is tailored to each individual based on the severity of symptoms, underlying venous pathology, and overall health status. A comprehensive evaluation by a healthcare professional specializing in vascular medicine or vascular surgery is important to determine the most appropriate treatment approach for each patient.
FAQ
Post-thrombotic syndrome (PTS) is a chronic condition that can persist for a long time and may be permanent. Treatment aims to alleviate symptoms, improve quality of life, and prevent further complications. Early diagnosis and timely intervention are key to preventing or minimizing the long-term effects of PTS. Working closely with a healthcare professional specializing in vascular medicine or vascular surgery can help manage the symptoms and improve overall outcomes.
Exercise is generally beneficial for individuals with post-thrombotic syndrome (PTS). Regular physical activity can help improve circulation, strengthen the muscles in the affected limb, reduce swelling, and alleviate some of the symptoms associated with PTS. Exercise can have several positive effects on individuals with PTS, such as improved blood flow, muscle pump activation, reduction of swelling, improved range of motion, and weight management. It is important to start slowly and gradually increase the intensity and duration of exercise to avoid overexertion and injury. Consult with a healthcare professional to determine the most suitable exercise regimen for your condition.
Post-thrombotic syndrome (PTS) can be exacerbated by several factors, such as prolonged immobility, lack of compression, obesity, recurrent DVT, failure to follow treatment plan, trauma or injury, smoking, and high impact activities. It is important for individuals with PTS to be aware of these aggravating factors and take appropriate measures to minimize their impact. Following the recommended treatment plan, maintaining a healthy lifestyle, wearing compression garments as prescribed, and avoiding prolonged immobility can help in managing and reducing the severity residual symptoms of PTS. Regular communication with your healthcare provider is essential to ensure appropriate management and address any concerns or changes in symptoms.