Our circulatory system is an intricate network of blood vessels, with arteries and veins playing distinct yet complementary roles. They might seem like simple tubes, but their structures are finely tuned to their specific functions in the body. Superficial veins, located close to the skin’s surface, contrast with deeper veins found in the muscles and play a crucial role in the circulatory system. Let’s dive into the fascinating world of these vessels and see what makes them unique. Understanding these differences is essential for maintaining optimal vascular health.
Overview of the Cardiovascular System
The cardiovascular system is a marvel of biological engineering, consisting of a vast network of blood vessels that are essential for maintaining the body’s overall health. This intricate system is composed of three main types of blood vessels: arteries, capillaries, and veins, all lined with endothelial cells. Each type plays a unique role in the circulatory process.
Arteries are responsible for transporting oxygen-rich blood from the heart to various tissues throughout the body. These vessels are designed to handle high pressure, ensuring that oxygen and nutrients are efficiently delivered to where they are needed most. On the other hand, veins carry oxygen-poor blood back to the heart. This return journey is crucial for reoxygenation and the removal of waste products from the body.
Capillaries, the smallest blood vessels, act as intermediaries between arteries and veins. They facilitate the exchange of oxygen, nutrients, and waste products between blood and tissues. The total length of blood vessels in an adult human is astonishing, stretching approximately 100,000 kilometers when laid end to end. This extensive network ensures that every cell in the body receives the necessary sustenance and can dispose of metabolic waste effectively.
General Organization
Characteristics of Arteries
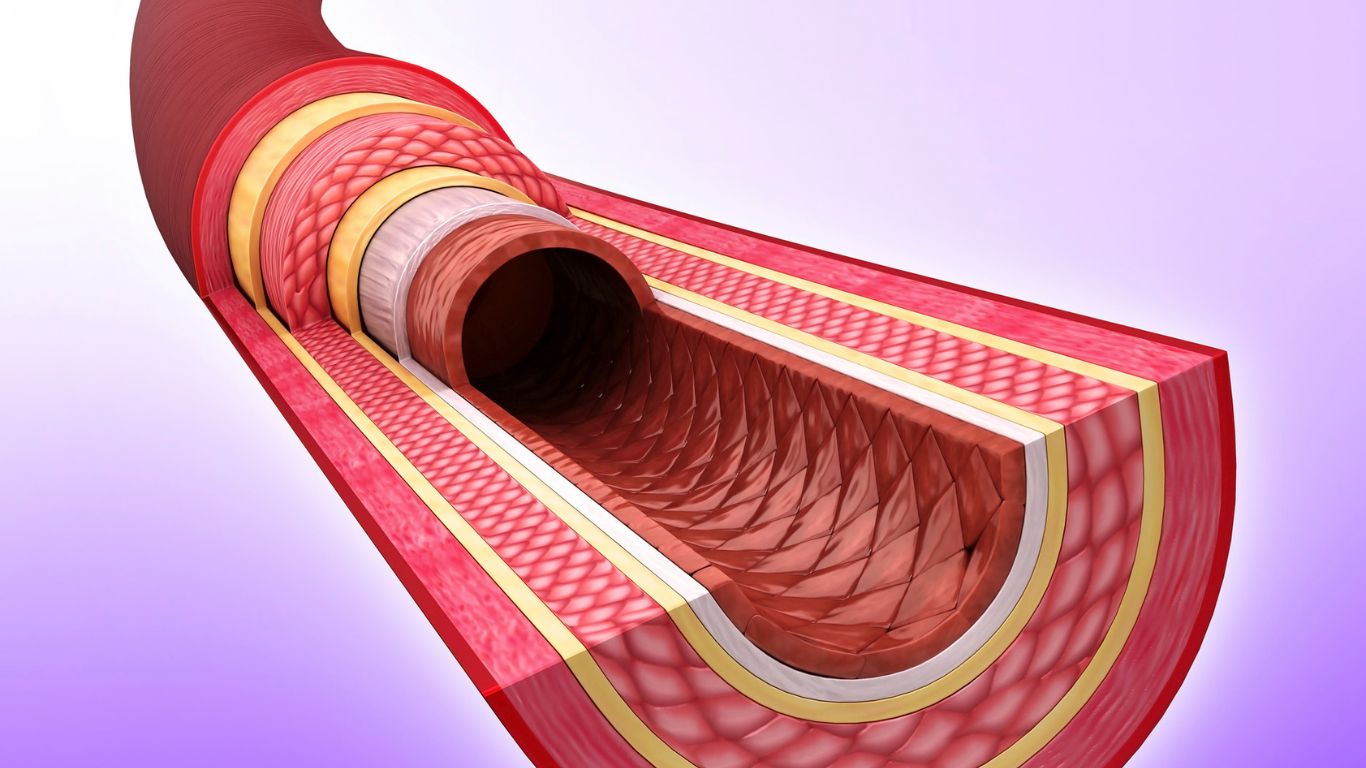
Arteries are blood vessels that play a crucial role in the circulatory system by transporting oxygen-rich blood from the heart to the rest of the body. These vessels are designed to withstand high blood pressure, thanks to their thick-walled structures. The walls of arteries are composed of three distinct layers:
Tunica Externa: The outer layer, made of connective tissue, provides structural support and protection.
Tunica Media: The middle layer, consisting of smooth muscle cells and elastic fibers, allows arteries to expand and contract with each heartbeat, ensuring smooth blood flow.
Tunica Intima: The innermost layer, lined with endothelium, reduces friction and facilitates the efficient movement of blood.
Arteries branch out into smaller vessels called arterioles and capillaries, which are essential for the exchange of oxygen and nutrients with the body’s tissues. By maintaining blood pressure and delivering oxygen-rich blood to tissues and organs, arteries play a vital role in sustaining life and supporting cellular function.
Why Are Arteries More Elastic Than Veins?
Arteries are designed to handle high pressure. Every time your heart beats, it sends a surge of blood through your arteries. This pressure is so strong that the artery walls need to be incredibly elastic and resilient. Their walls contain a thick layer of smooth muscle, elastic fibers, and collagen fibers, allowing them to expand and contract with each heartbeat. The smooth muscle cells in the tunica media play a crucial role in regulating vessel wall tension and arterial pressure, which helps maintain a consistent flow of blood and smoothens out the pulses, ensuring that oxygen-rich blood reaches every part of the body efficiently.
How Do Artery Walls Compare to Vein Walls?
In contrast, veins don’t deal with the same high pressure as arteries. After blood has delivered its oxygen to tissues and is making its way back to the heart, it travels at a much lower pressure. As a result, veins have thinner walls with less muscle and elastic tissue, including a reduced presence of smooth muscle cells compared to artery walls. Instead of the thick, muscular walls found in arteries, veins rely on other mechanisms—like valves—to move blood back to the heart, often working against gravity, especially in the legs. Venous return is crucial in this process, as it refers to the flow of blood back to the heart, ensuring that the circulatory system functions effectively.
Characteristics of Veins
Veins are blood vessels that are responsible for transporting oxygen-poor blood back to the heart. Unlike arteries, veins have thinner walls and are less muscular, making them more prone to stretching and twisting. The structure of veins includes three layers:
Tunica Externa: The outer layer, composed of connective tissue, provides support and protection.
Tunica Media: The middle layer, containing smooth muscle cells, is thinner than in arteries, reflecting the lower pressure in veins.
Tunica Intima: The innermost layer, lined with endothelium, ensures smooth blood flow.
Veins have a larger diameter than arteries and are equipped with one-way valves that prevent blood from flowing backward. These valves are crucial for maintaining unidirectional blood flow, especially in the limbs where blood must be pushed against gravity to return to the heart. By collecting oxygen-poor blood from tissues and organs and ensuring its return to the heart, veins play an essential role in the circulatory system.
The Three Layers of a Vein Wall
Both arteries and veins have three main layers in their walls:
Tunica Intima: The innermost layer, which is smooth to help blood flow easily.
Tunica Media: The middle layer, which contains smooth muscle cells and elastic fibers. The smooth muscle cells play a crucial role in regulating vessel wall tension and arterial pressure by contracting and relaxing, which impacts the diameter of arterioles and consequently affects blood flow in capillary beds. This layer is much thinner in veins compared to arteries.
Tunica Externa (Adventitia): The outer layer, which provides structural support and contains connective tissue, nerves, and small blood vessels to nourish the larger vessel walls.
Why Do Arteries Have Thick Walls and Veins Have Thin Walls?
The thick walls of arteries are essential to withstand and regulate the high pressure exerted by the heart. This robust structure, composed of smooth muscle cells, helps control blood flow by constricting or dilating, which adjusts blood pressure and distribution. On the other hand, veins have thin walls because they operate under low pressure. Instead of relying on thick muscle layers, they use valves to prevent backflow and assist blood return to the heart.
Vascular resistance plays a crucial role in regulating blood flow by determining how much resistance the blood encounters as it travels through the vessels.
Veins Have Valves—Why?
Unlike arteries, veins have to push blood back to the heart, often working against gravity, especially in the lower body. Superficial veins, located close to the skin’s surface, play a crucial role in the circulatory system and are equipped with valves to prevent blood pooling. To prevent blood from pooling or flowing backward and to manage venous pressure, veins are equipped with one-way valves. These valves act like little gates, ensuring that blood flows only in one direction—toward the heart. This is why you’ll often hear about issues like varicose veins, where the valves fail to function properly, leading to blood pooling and vein swelling.
How Do Arteries, Veins, and Capillaries Compare?
Capillaries are the tiny blood vessels where the exchange of oxygen, nutrients, and waste products occurs between blood and tissues. They connect the arterial and venous systems, forming a bridge between arteries and veins. While arteries have thick walls to withstand high pressure, containing smooth muscle cells in the tunica media to regulate vessel wall tension and arterial pressure, veins have valves to assist low-pressure flow. Capillaries, on the other hand, have walls that are just one cell thick to allow for easy exchange of substances. Microcirculation, which involves the flow of blood through the smallest vessels including capillaries, is crucial for the efficient exchange of substances between blood and tissues.
Why Do Arteries Pulsate but Veins Don’t?
Arteries pulsate because they are directly connected to the pumping action of the heart, which creates a rhythmic, palpable pulse as the blood surges through them. The presence of smooth muscle cells in the arterial walls plays a crucial role in this pulsating action by regulating vessel wall tension and arterial pressure. Veins, on the other hand, carry blood back to the heart at a much steadier, lower pressure, without the pulsating force. Hemodynamics, the study of blood flow, explains how the dynamic pressure changes within arteries contribute to their pulsating nature.
Can You Feel a Pulse in Both Veins and Arteries?
You can typically feel a pulse only in arteries, not veins. This is because the pulse is the result of the heart’s forceful pumping action, which is transmitted through the elastic walls of arteries and regulated by the contraction of smooth muscle cells. Veins, lacking this force, don’t create a palpable pulse. Vascular compliance, the ability of blood vessels to expand and contract, plays a crucial role in maintaining proper blood flow and pressure within the circulatory system.
How Do Arteries and Veins Get Energy?
Arteries and veins have their own tiny blood vessels called the vasa vasorum that supply their outer layers with nutrients and oxygen. Smooth muscle cells in the tunica media also rely on the vasa vasorum for essential nutrients, oxygen, and nutrient exchange. This is crucial for maintaining the health of the vessel walls, especially in larger arteries and veins.
What Happens When Blood Travels from Arteries to Veins?
As blood moves through the arterial system, it travels to the capillaries, where it delivers oxygen and nutrients to tissues and picks up waste products. Smooth muscle cells in the tunica media of arterioles regulate vessel wall tension and arterial pressure, impacting the diameter of arterioles and consequently affecting blood flow in capillary beds. It then flows into the venous system to be returned to the heart and lungs for oxygenation. This journey from high-pressure arteries to low-pressure veins is essential for maintaining efficient circulation and proper organ function. Venous return, the process of blood returning to the heart, is crucial for sustaining the circulatory system’s efficiency and ensuring that deoxygenated blood is reoxygenated.
Blood Flow Differences Between Arteries and Veins
The flow of blood through arteries and veins differs significantly due to their distinct structures and functions within the circulatory system. Smooth muscle cells in the tunica media of arteries play a crucial role in regulating arterial pressure by controlling the diameter of arterioles, which in turn affects blood flow in capillary beds and responds to the metabolic needs of tissues. Vascular resistance, the resistance that must be overcome to push blood through the circulatory system, is a key factor in regulating blood flow. Here’s a breakdown of these differences:
1. Direction of Blood Flow
Arteries: Carry oxygenated blood away from the heart to the body’s tissues, with the exception of the pulmonary arteries, which carry deoxygenated blood to the lungs.
Veins: Return deoxygenated blood toward the heart, except for the pulmonary veins, which carry oxygenated blood from the lungs back to the heart. Venous return is the process of blood flowing back to the heart, which is crucial for maintaining blood circulation and ensuring that the heart has enough blood to pump.
2. Blood Pressure
Arteries: Blood flow in arteries is under high pressure, generated by the forceful pumping of the heart. This pressure helps propel blood throughout the body.
Veins: Blood pressure in veins is much lower. The flow relies on venous pressure, skeletal muscle contractions, valves within the veins, and pressure changes in the chest during breathing to push blood back to the heart.
3. Flow Characteristics
Arteries: Blood flows in pulses, corresponding to the heartbeats, creating a rhythmic surge that can be felt as a pulse in certain areas of the body, such as the wrist or neck. Vascular compliance, which is the ability of blood vessels to expand and contract, plays a crucial role in maintaining proper blood flow and pressure within the circulatory system.
Veins: Blood flows steadily and continuously, without the pulsing seen in arteries. This is because the pressure exerted by the heart has significantly diminished by the time blood reaches the veins.
4. Wall Structure and Blood Flow Speed
Arteries: Have thick, elastic, and muscular walls to withstand and regulate the high-pressure blood flow. The elasticity and collagen fibers help maintain continuous blood flow between heartbeats.
Veins: Have thinner, less muscular walls as they don’t need to withstand high pressure. The flow speed is slower compared to arteries, and veins often have valves to prevent backflow, particularly in the limbs.
5. Presence of Valves
Arteries: Do not have valves because the high pressure of blood flow prevents backflow.
Veins: Contain one-way valves that prevent the backward flow of blood, especially in the legs, where blood must be pushed against gravity to return to the heart. This process is known as ‘venous return’ and is crucial for maintaining proper circulation and ensuring that deoxygenated blood is efficiently transported back to the heart.
6. Color and Oxygen Content
Arteries: Typically carry bright red, oxygen-rich blood, except for the pulmonary arteries, which carry dark red, deoxygenated blood. Nutrient exchange is a crucial process in the circulatory system, where blood vessels deliver essential nutrients to tissues and remove waste products.
Veins: Carry dark red, deoxygenated blood (appearing blue through the skin) back to the heart, except for the pulmonary veins, which carry oxygenated blood.
7. Function in the Circulatory System
Arteries: Distribute oxygen and nutrients to all parts of the body, supporting cellular function.
Veins: Collect and transport waste products and carbon dioxide from tissues back to the heart and lungs for removal and re-oxygenation.
Maintaining vascular health is crucial for the proper function of the circulatory system, ensuring efficient blood flow and nutrient delivery.
Why Are Veins Superficial and Arteries Deep?
Veins, including superficial veins located close to the skin’s surface, facilitate the return of blood to the heart and help regulate body temperature. Arteries, on the other hand, are deeper to protect them from injury, as they carry oxygen-rich blood under high pressure that’s crucial for survival. Vascular resistance plays a key role in this protection by helping to regulate blood flow and pressure within the arteries.
Clinical Significance of Vein Structure
Deep Veins and Blood Flow
Deep veins are blood vessels located deep within the muscles of the arms and legs, playing a pivotal role in maintaining efficient blood flow. These veins are tasked with carrying oxygen-poor blood back to the heart, a journey that requires overcoming the challenge of gravity, especially from the lower extremities. To facilitate this process, deep veins are equipped with one-way valves that prevent blood from flowing backward, ensuring a steady, unidirectional flow towards the heart. Venous return, the process of blood returning to the heart, is essential for maintaining proper circulation and the overall function of deep veins.
However, the functionality of these veins can be compromised by conditions such as deep vein thrombosis (DVT). DVT occurs when blood clots form in the deep veins, often in the legs. This condition can be life-threatening if a clot dislodges and travels to the lungs, causing a pulmonary embolism. Such an event can obstruct blood flow to the lungs, leading to severe complications or even death. Therefore, understanding the structure and function of deep veins is crucial for recognizing and preventing conditions like DVT.
Varicose Veins and Their Impact
Varicose veins are a common condition that affects millions of people worldwide, characterized by veins that have become enlarged and twisted. This occurs when the vein walls weaken and stretch, causing blood to pool and flow backward. Increased venous pressure also contributes to the development of varicose veins. The result is often visible, swollen veins that can cause discomfort and cosmetic concerns.
The symptoms of varicose veins can range from mild to severe, including swelling, pain, and skin discoloration. In some cases, varicose veins can lead to more serious conditions such as chronic venous insufficiency. This occurs when the veins are unable to pump blood effectively, leading to persistent swelling and pain in the legs. Additionally, varicose veins can increase the risk of developing blood clots, which can potentially lead to a pulmonary embolism if the clot travels to the lungs.
Understanding the impact of varicose veins and the importance of vein health can help in managing symptoms and preventing complications. Regular exercise, maintaining a healthy weight, and avoiding prolonged periods of standing or sitting can all contribute to better vein health and reduce the risk of developing varicose veins.
Prevention and Treatment of Vein Disorders
Maintaining healthy veins is vital for overall circulatory health. Here are some practical tips for preventing and managing vein disorders:
Regular Exercise: Engaging in physical activities like walking, swimming, or cycling can improve blood flow and reduce the risk of varicose veins.
Balanced Diet: Eating a diet rich in fruits, vegetables, and whole grains supports vein health and overall circulation.
Avoid Prolonged Sitting or Standing: Taking breaks to move around can prevent blood from pooling in the legs.
Compression Stockings: Wearing compression stockings can help improve blood flow and reduce the risk of varicose veins.
Elevate Your Legs: Elevating your legs can reduce swelling and improve blood flow.
Avoid Crossing Legs or Ankles: This can reduce pressure on the veins and promote better circulation.
For those already experiencing vein disorders, several treatment options are available:
Sclerotherapy: A procedure where a solution is injected into the vein, causing it to collapse and fade.
Laser Therapy: Uses laser energy to close off varicose veins.
Vein Stripping: Surgical removal of damaged veins.
In severe cases, surgery may be necessary to repair or remove damaged veins. By following these preventive measures and seeking appropriate treatment, individuals can manage symptoms and improve their vein health, reducing the risk of complications like chronic venous insufficiency and blood clots. Regular exercise and a healthy diet remain foundational practices for maintaining overall circulatory health.
What are 3 major veins?
The three major veins in the human body are:
Superficial veins, located close to the skin’s surface, play a crucial role in the venous system by aiding blood circulation and returning deoxygenated blood to the heart. Damage to these veins can lead to venous disease, affecting blood flow and potentially causing serious health risks. Venous return is the process of blood flowing back to the heart through these veins, which is essential for maintaining proper circulation and overall cardiovascular health.
1. Superior Vena Cava
The superior vena cava is a large vein that carries deoxygenated blood from the upper half of the body, including the head, neck, chest, and upper limbs, back to the right atrium of the heart. It is one of the primary veins responsible for returning blood to the heart for reoxygenation.
2. Inferior Vena Cava
The inferior vena cava is the largest vein in the body and carries deoxygenated blood from the lower half of the body, including the abdomen, pelvis, and lower limbs, back to the right atrium of the heart. Like the superior vena cava, it plays a crucial role in returning blood to the heart.
3. Jugular Veins
The jugular veins consist of the internal and external jugular veins, which drain blood from the head, brain, face, and neck back to the heart via the superior vena cava. The internal jugular vein is the more significant of the two, carrying blood from the brain and deep structures of the head and neck.
These veins are essential components of the venous system, ensuring that deoxygenated blood is efficiently returned to the heart for reoxygenation and circulation throughout the body.
Final Thoughts
Arteries and veins may seem like simple vessels, but their unique structures are essential for our bodies to function correctly. Superficial veins, located close to the skin’s surface, play a crucial role in the circulatory system by aiding in blood flow and preventing complications. From the thick, muscular walls of arteries to the thin, valve-equipped walls of veins, each vessel is perfectly adapted to its role. Understanding these differences helps us appreciate how intricately designed our circulatory system is, keeping blood flowing smoothly and efficiently throughout our bodies. Maintaining vascular health is crucial for the proper function of the circulatory system.