The recurring problem
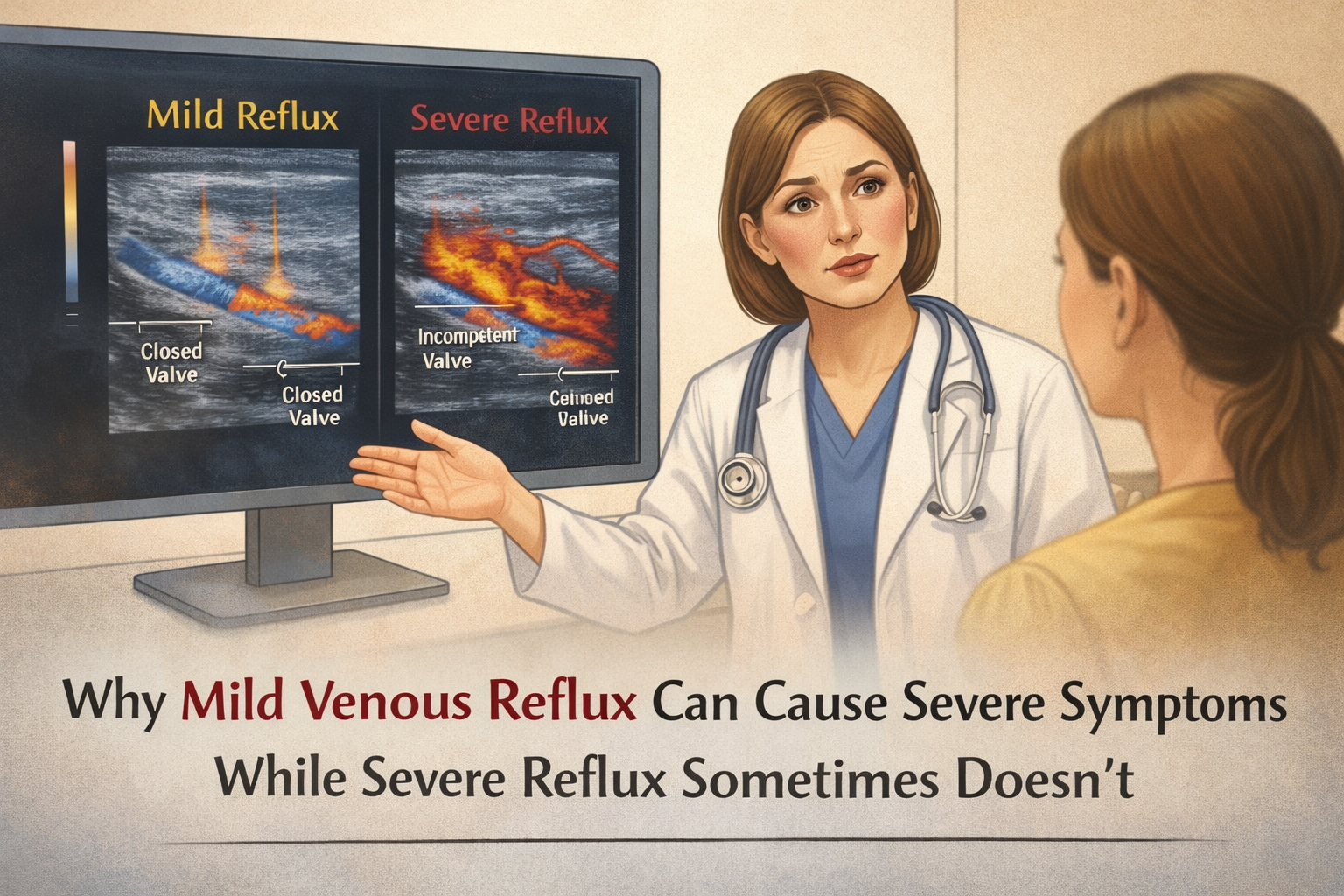
In venous disease, there is a familiar and often confusing pattern: patients with “mild” venous reflux on ultrasound may report significant pain, heaviness, swelling, burning, or fatigue, while others with clearly severe reflux—long reflux times, multiple incompetent segments, or advanced anatomical changes—report relatively few symptoms.
This mismatch can leave patients feeling unheard and clinicians unsure how to reconcile imaging with lived experience. Yet this pattern is not unusual, and it does not imply exaggeration, poor coping, or inaccurate testing. It reflects how venous symptoms are generated and perceived, not just how abnormal the veins look.
Why this happens
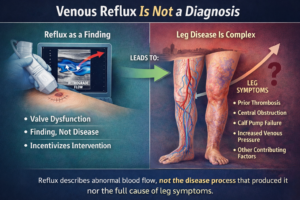
1) Venous reflux severity on imaging does not equal symptom severity
Duplex ultrasound measures flow direction, reflux duration, and vein anatomy. These metrics describe hemodynamics, not discomfort.
Symptoms arise from tissue response, including pressure changes, inflammation, microcirculatory stress, and nerve activation. Two people with similar reflux measurements can therefore feel very different.
In venous disease, what the tissue experiences matters more than what the vein looks like.
2) Early venous disease can be more symptomatic
Paradoxically, people with mild or early venous reflux often report stronger symptoms. Several mechanisms may explain this:
Veins and surrounding tissues are still reactive and dynamic
Pressure changes fluctuate throughout the day rather than remaining constant
Valvular dysfunction may be intermittent, creating variable venous hypertension
This variability can produce sensations of aching, throbbing, tightness, or burning that feel intense—even when reflux duration appears limited on a snapshot study.
3) The role of sensory nerves and mechanoreceptors
Veins and perivascular tissues are richly innervated. When venous pressure rises, even modestly, it can activate:
Stretch-sensitive mechanoreceptors
Perivascular sensory nerves
Inflammatory signaling pathways
In some individuals, these sensory systems are more responsive or more easily sensitized, meaning smaller pressure changes produce disproportionate symptoms. This helps explain why symptoms may precede visible skin changes or significant varicosities.
4) Chronic severe reflux can dull sensation over time
In contrast, long-standing or severe venous reflux may lead to neural adaptation.
With persistent venous hypertension:
Nerves may become less responsive
Sensation can shift from pain to heaviness or even relative numbness
Symptoms may feel “stable” or less intrusive, despite progressive disease
This does not indicate benign disease—it indicates that the body has adjusted to ongoing abnormal pressure.
5) Microcirculation and inflammation matter more than reflux time alone
Venous symptoms are strongly influenced by what happens at the capillary and tissue level:
Capillary leakage
Local inflammation
Interstitial edema
Tissue hypoxia
Mild reflux that disproportionately affects microcirculation can cause pain, swelling, or skin sensitivity, while more severe reflux confined to larger veins may cause fewer immediate sensory symptoms.
6) Posture, muscle pump function, and daily exposure shape symptoms
Venous reflux measurements are typically obtained in controlled conditions. Real life is different.
Symptoms depend on:
Time spent standing or sitting
Calf muscle pump efficiency
Occupation and activity patterns
Compression use and leg elevation habits
A person with mild reflux but high daily venous load may feel worse than someone with severe reflux who moves frequently or has adapted physiologically.
The cost of delay
Clinical cost
When symptom severity is discounted due to “mild” imaging findings:
Early venous disease may go undertreated
Pain may be attributed to musculoskeletal or nonspecific causes
Opportunities for early intervention may be missed
Symptoms may progress before visible disease develops
Institutional cost
At a systems level, this mismatch can lead to:
Repeated consultations with inconclusive explanations
Delays in referral to vein doctors
Underutilisation of conservative therapies such as compression or exercise
Patient dissatisfaction despite technically accurate testing
Personal cost
For patients, the impact can include:
Feeling dismissed or minimized
Ongoing leg discomfort affecting work and mobility
Reduced activity levels and quality of life
Loss of confidence in diagnostic results that do not match lived experience
Venous symptoms are not imaginary—and they are not always proportional to ultrasound findings.
What remains uncertain
There are important uncertainties in venous disease assessment:
Which patients with mild reflux will remain stable and which will progress
How individual nerve sensitivity influences symptom perception
How well a single ultrasound captures daily venous stress
Why some tissues adapt while others remain highly symptomatic
Acknowledging this uncertainty allows for more flexible, patient-centered care.
A more useful way to think about venous reflux symptoms
When mild venous reflux causes major symptoms, it is often because early disease is dynamic, sensory-driven, and tissue-responsive. When severe reflux causes few symptoms, it may reflect adaptation rather than absence of harm.