Leg vein issues are more than just a cosmetic concern. For many people, vein disorders, including venous disease, can cause significant discomfort and lead to more serious health complications if left untreated. If you experience pain, swelling, or heaviness in your legs, it could be a sign of a vein disorder. Understanding the symptoms and seeking treatment early from a vein specialist can prevent the condition from worsening and improve your quality of life.
In this blog, we’ll explore the common symptoms of vein disorders and when to seek help from a vein doctor.
Understanding Vein Disorders and Chronic Venous Insufficiency
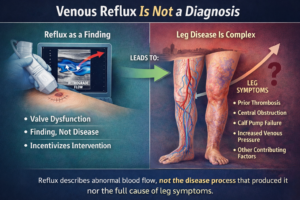
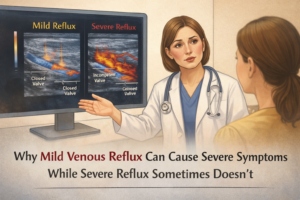
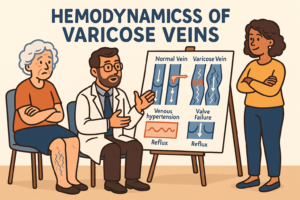
Vein disorders occur when your veins are unable to efficiently return blood to the heart. This often happens when the valves in the veins, particularly in the legs, weaken or become damaged. As a result, blood pools in the veins, causing them to enlarge, bulge, or twist, leading to conditions like varicose veins, spider veins, and chronic venous insufficiency (CVI).

What is Chronic Venous Insufficiency?
Chronic venous insufficiency (CVI) is a condition where the veins in your legs are unable to efficiently return blood to the heart. This happens when the valves in the leg veins, which help regulate blood flow, become damaged or weakened. As a result, blood pools in the legs, leading to increased pressure in the veins. This can cause a range of symptoms, including pain, swelling, and changes in skin color or texture. CVI can affect any of the leg veins, including the superficial veins, which are close to the skin’s surface, and the deep veins, which are located deeper within the leg muscles. If left untreated, CVI can lead to more serious complications, such as venous ulcers or chronic pain.
Common Symptoms of Vein Disorders
If you’re experiencing discomfort in your legs, here are some common symptoms that may indicate a vein disorder:
1. Pain or Aching in the Legs
A dull, aching pain in the legs, especially after prolonged periods of standing or sitting, can be a sign of a vein disorder. This discomfort may feel like heaviness or a throbbing sensation in your legs.
Why it happens: The pooling of blood in damaged veins increases pressure, which can lead to pain or discomfort, particularly in the lower legs.
2. Swelling in the Legs or Ankles
Swelling (edema) is a common symptom of venous insufficiency. It often occurs at the end of the day, especially if you’ve been standing or sitting for extended periods.
Why it happens: Poor circulation causes blood to accumulate in the lower legs, leading to fluid buildup and swelling.
3. Itching Around the Veins
Itchy skin around the affected veins can be an early sign of venous insufficiency or varicose veins. This itching is often accompanied by dry or irritated skin.
Why it happens: Blood pooling in the veins can cause inflammation, leading to skin irritation and itchiness.
4. Heaviness or Fatigue in the Legs
Many people with vein disorders report feeling a sense of heaviness or fatigue in their legs, particularly after physical activity. This sensation can make walking or standing for long periods difficult.
Why it happens: Damaged veins struggle to pump blood efficiently, causing a buildup of pressure and leading to feelings of heaviness or fatigue in the legs.
5. Visible Varicose or Spider Veins
Varicose veins are enlarged, bulging veins that are often visible under the skin. Spider veins are smaller, web-like veins that can appear on the surface of the skin.
Why it happens: Weak or damaged valves in the veins allow blood to flow backward, causing the veins to enlarge or become twisted.
6. Cramping or Restless Legs
Cramping in the legs, particularly at night, can be a symptom of vein disorders. Some people may also experience restless leg syndrome, where they feel the need to move their legs to relieve discomfort.
Why it happens: Poor circulation caused by venous insufficiency can lead to muscle cramps, particularly when you’re inactive or lying down.
7. Skin Discoloration or Ulcers
In more advanced cases of vein disorders, you may notice changes in skin color around the ankles or lower legs. This can range from redness to a brownish discoloration. In severe cases, venous ulcers (open sores) may develop.
Why it happens: Chronic venous insufficiency causes poor blood flow, which can damage the skin and underlying tissues, leading to discoloration or sores that take a long time to heal.
What Causes Vein Disorders, Including Deep Vein Thrombosis?
Several factors can contribute to the development of vein disorders. Some of the most common risk factors include:
Prolonged standing or sitting: Jobs that require you to stay on your feet or sit for long periods can increase your risk.
Age: The risk of vein disorders increases with age, as veins naturally lose elasticity over time.
Family history: Genetics play a significant role, and if you have a family history of varicose veins or other vein disorders, your risk is higher.
Pregnancy: Hormonal changes during pregnancy can weaken vein walls and increase the risk of developing varicose veins.
Obesity: Excess weight puts additional pressure on your leg veins, which can lead to vein disorders.
Lack of exercise: Physical inactivity can slow blood circulation, leading to venous insufficiency.
A blood clot forming in a deep vein, known as deep vein thrombosis (DVT), can lead to complications such as post-thrombotic syndrome.
Diagnosing Vein Disorders
Diagnosing vein disorders involves a comprehensive approach that includes taking a detailed medical history, performing a physical examination, and conducting diagnostic tests. Your healthcare provider will start by asking about your symptoms, lifestyle, and any family history of vein disorders, such as varicose veins or previous blood clots. During the physical examination, the doctor will look for visible signs of vein disorders, such as swelling, skin changes, or the presence of varicose veins. This initial assessment helps identify potential risk factors and guides the selection of appropriate diagnostic tests.
Diagnostic Tests
Several diagnostic tests can help confirm the presence of vein disorders and determine their severity:
Duplex Ultrasound: This non-invasive test uses sound waves to create detailed images of your veins and assess blood flow. It is particularly useful for diagnosing conditions like deep vein thrombosis (DVT) and chronic venous insufficiency. The ultrasound can show if there are any blood clots or if the veins are functioning properly.
Venogram: In this test, a contrast dye is injected into the veins, and X-rays are taken to visualize the veins and blood flow. This helps identify any blockages or abnormalities in the veins.
Blood Tests: Blood tests can detect markers of blood clots or other underlying conditions that may contribute to vein disorders. These tests are often used in conjunction with imaging studies to provide a comprehensive diagnosis.
Treating Vein Disorders
Treating vein disorders depends on the severity of the condition and the individual’s overall health. A combination of lifestyle changes, compression stockings, and minimally invasive procedures can effectively manage symptoms and improve blood flow.
Treatment Options
Lifestyle Changes: Adopting healthier habits can significantly improve vein health. Losing weight, exercising regularly, and elevating your legs can enhance blood flow and reduce symptoms. Simple activities like walking or swimming can make a big difference.
Compression Stockings: Wearing compression stockings helps improve blood flow and reduce swelling. These specially designed stockings apply gentle pressure to your legs, encouraging blood to move more efficiently. They come in various compression levels and can be worn throughout the day.
Minimally Invasive Procedures: For more severe cases, minimally invasive procedures like endovenous laser ablation or radiofrequency ablation (RFA) can be used to close off affected veins and improve blood flow. These procedures are performed on an outpatient basis and involve minimal downtime.
Sclerotherapy: This treatment involves injecting a chemical solution into the affected vein, causing it to collapse and eventually be absorbed by the body. Sclerotherapy is effective for treating smaller varicose veins and spider veins.
Surgery: In severe cases where other treatments are not effective, surgery may be necessary to remove the affected vein or repair damaged valves. Surgical options are typically reserved for advanced vein disorders that significantly impact quality of life.
When to See a Vein Doctor
If you’re experiencing any of the symptoms mentioned above, it’s important to consult a vein doctor for an evaluation. Vein disorders are progressive, meaning they can worsen over time if left untreated. Early treatment can alleviate symptoms, prevent complications, and improve your leg health.
It is crucial to treat varicose veins as they can pose significant medical issues that may worsen over time and lead to serious complications.
A vein doctor will assess your condition and recommend the most appropriate treatment based on the severity of your symptoms. Some common treatments for vein disorders include:
Sclerotherapy: A minimally invasive treatment that involves injecting a solution into the affected veins to collapse and close them.
Endovenous Laser Treatment (EVLT): A laser is used to heat and seal varicose veins from the inside.
Radiofrequency Ablation (RFA): Similar to EVLT, this procedure uses radiofrequency energy to close off varicose veins.
Compression Stockings: These specially designed stockings help improve circulation and reduce swelling and discomfort.
Conclusion
If your leg veins are causing you pain or discomfort, you may be dealing with a vein disorder that requires medical attention. From varicose veins to venous insufficiency, these conditions can affect your daily life if left untreated. Consulting a vein doctor is the first step toward understanding the cause of your symptoms and finding an effective treatment plan. With the right care, you can relieve your discomfort and improve your overall vein health.
At Laurel Clinical, we have experience in diagnosing and treating vein disorders with advanced, minimally invasive techniques. Contact us today to schedule a consultation and take the first step toward healthier, pain-free legs.