Platelet Rich Plasma in Chronic Venous Ulcers
Venous ulcers (VUs) are a significant public health issue, representing around 70% of lower limb ulcers. They are not only challenging to treat but also come with a high recurrence rate. Chronic leg ulcers impact patients’ quality of life, often leading to pain, immobility, and, in severe cases, infection and hospitalisation. Traditional treatment options, such as dressings and debridement, may not provide the necessary healing environment, especially for ulcers that remain stuck in the inflammatory phase of the wound healing process.
In recent years, Platelet-Rich Plasma (PRP) has gained attention as a promising treatment for chronic ulcers, including venous ulcers. By harnessing the body’s natural healing processes, PRP therapy introduces high concentrations of growth factors directly to the ulcer site, helping to accelerate wound healing and improve outcomes. This blog will explore the role of PRP in treating leg ulcers, its benefits, and how it compares to other therapies like Platelet-Rich Fibrin (PRF).

The Challenges of Treating Venous Ulcers
Venous ulcers develop as a result of poor blood circulation in the lower extremities, typically due to chronic venous insufficiency. When the veins in the legs are unable to return blood efficiently to the heart, it leads to increased pressure in the veins, causing damage to the skin and tissue. This results in ulcers, which are often slow to heal and highly susceptible to infection.
Treating venous ulcers is challenging for several reasons:
1. Chronic nature: Venous ulcers often become chronic due to the body’s inability to efficiently heal the damaged tissue.
2. High recurrence rate: Even when treated, venous ulcers have a high likelihood of recurring, as the underlying vascular issues may remain unresolved.
3. Limited treatment options: Standard treatments, such as compression therapy and wound care, often fail to address the complex healing needs of these ulcers.
Venous Ulcer Insights
Chronic venous leg ulcers (CVLUs) result from chronic venous insufficiency, a condition where weakened or damaged vein valves fail to maintain proper blood flow to the heart. This causes blood to pool in the legs, increasing pressure and leading to tissue damage and ulceration. Risk factors for CVLUs include aging, as vein function naturally declines over time; varicose veins, which predispose individuals to venous insufficiency; and conditions like deep vein thrombosis (DVT) that damage vein walls and valves. Lifestyle factors such as prolonged standing or sitting, obesity, and a family history of venous disease also significantly increase the risk of developing these ulcers.
Symptoms of CVLUs include slow-healing wounds, typically near the ankle, accompanied by swelling, discoloration, pain, itching, and hardened skin around the ulcer site. Preventive measures are key to managing and reducing the recurrence of venous ulcers. Regular use of compression stockings helps improve circulation, while avoiding prolonged immobility and elevating the legs reduce venous pressure. Moisturizing the skin prevents cracking and dryness, further lowering the risk of ulcer formation. Proactive care and early intervention can effectively manage CVLUs and improve long-term leg health.
Treatment Options for Chronic Venous Leg Ulcers
The primary goals of treatment for chronic venous leg ulcers are to reduce venous pressure, promote healing, and prevent infection. There are several treatment options available, ranging from traditional wound care to more advanced therapies like Platelet-Rich Plasma (PRP) therapy.
1. Compression Therapy
Compression therapy is considered the cornerstone of venous ulcer treatment. It involves the use of compression stockings, bandages, or wraps to apply pressure to the legs, improving blood circulation and reducing swelling. Compression therapy helps prevent blood from pooling in the lower extremities and promotes the healing of the ulcer by enhancing blood flow back to the heart.
For compression therapy to be effective, it must be used consistently and correctly. Your healthcare provider will determine the appropriate level of compression based on the severity of your venous insufficiency and ulcer.
2. Wound Care and Dressings
Proper wound care is essential for promoting healing and preventing infection. This includes:
Cleansing the wound: Keeping the wound clean helps prevent infection and promotes healing. Mild, non-irritating solutions are typically used for cleaning.
Debridement: This process involves removing dead or damaged tissue from the ulcer to encourage healthy tissue growth.
Dressings: Special dressings are used to protect the ulcer, maintain a moist wound environment, and promote healing. Some dressings are infused with medications like antibiotics or silver, which have antimicrobial properties.
3. Medications
Antibiotics: If the ulcer becomes infected, oral or topical antibiotics may be prescribed to treat the infection.
Pentoxifylline: This medication improves blood flow and may be used alongside compression therapy to enhance healing.
Pain relief: Over-the-counter or prescription pain medications may be recommended to alleviate discomfort.

Advanced therapies
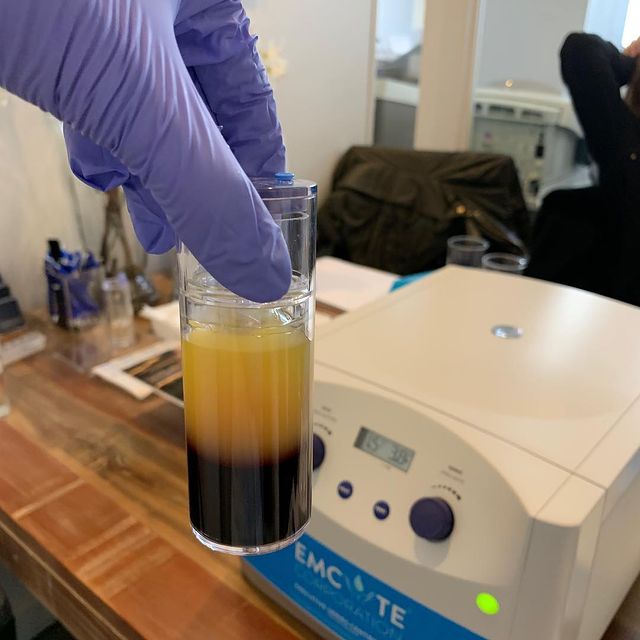
Platelet-Rich Plasma (PRP) therapy is an emerging treatment for chronic venous leg ulcers that harnesses the body’s natural healing processes. Clinical studies have demonstrated that the application of autologous platelet rich plasma gel significantly improves wound healing outcomes in chronic non-healing ulcers, particularly in patients with diabetic foot ulcers. PRP is derived from the patient’s own blood and contains a high concentration of platelets, which are rich in growth factors. These growth factors play a critical role in tissue regeneration, promoting cell proliferation, collagen formation, and wound healing.
PRP is injected directly into the ulcer site, delivering a concentrated dose of growth factors to accelerate the healing process. It has shown promise in speeding up healing times and improving outcomes in patients with chronic ulcers that have not responded to traditional treatments.
Surgical intervention
In cases where the venous ulcer is large or not responding to conventional treatments, skin grafts or surgical intervention may be necessary. Skin grafts involve transplanting healthy skin from another part of the body to cover the ulcer, promoting healing. Surgery may also be considered to improve venous circulation or remove damaged veins that contribute to ulcer formation.
Autologous Platelet Rich Plasma (PRP)
Autologous Platelet-Rich Plasma (PRP) is a cutting-edge medical treatment that leverages your body’s natural healing processes to promote tissue regeneration and repair. “Autologous” means that the treatment is derived from your own body, which makes it a safe and personalized therapy. PRP has gained widespread popularity in various fields of medicine, including dermatology, orthopedics, and sports medicine, due to its effectiveness in accelerating healing and minimizing the risk of adverse reactions.
PRP contains a high concentration of growth factors, including:
-
Platelet-Derived Growth Factor (PDGF): Stimulates cell growth, tissue regeneration, and blood vessel formation.
-
Vascular Endothelial Growth Factor (VEGF): Promotes the formation of new blood vessels, which helps improve circulation and bring nutrients to the affected tissue.
-
Transforming Growth Factor-Beta (TGF-β): Regulates inflammation and promotes the healing of damaged tissue by encouraging collagen production.
-
Insulin-Like Growth Factor (IGF): Supports cell growth and regeneration.
These growth factors are naturally present in the blood and play a critical role in healing injuries. By concentrating these factors in the PRP solution and injecting them into the damaged tissue, PRP therapy enhances the body’s ability to heal and regenerate faster.
When injected into the target area, such as an injured tendon, joint, or wound, PRP initiates a healing response that helps repair damaged tissues, reduce inflammation, and promote cell proliferation. Because PRP is derived from the patient’s own blood, the risk of rejection, allergic reactions, or adverse side effects is minimal.
Benefits of Autologous PRP Therapy
PRP therapy offers several key benefits that make it an attractive option for patients seeking non-invasive, natural treatments:
- Promotes Faster Healing: PRP enhances the body’s ability to repair damaged tissues by delivering concentrated growth factors to the affected area. This leads to faster healing of wounds, injuries, and damaged tissues.
- Safe and Natural Treatment: Since PRP is derived from the patient’s own blood, there is no risk of allergic reactions, infections, or transmission of diseases. It’s a completely natural treatment that uses the body’s own resources to promote healing.
- Minimally Invasive: PRP therapy involves a simple blood draw and injection, making it a minimally invasive procedure. There’s no need for surgery or long recovery times.
Reduces Pain and Inflammation: PRP has been shown to reduce pain and inflammation in conditions like osteoarthritis, tendon injuries, and chronic wounds, providing relief for patients who want to avoid or delay surgery.
Versatile Treatment: PRP can be used to treat a wide range of conditions, including joint pain, hair loss, skin rejuvenation, and chronic wounds. Its versatility makes it a popular option in multiple medical fields.
Future Directions and Research Needs
While the benefits of autologous platelet-rich plasma (PRP) in treating chronic venous leg ulcers are becoming increasingly evident, further research is essential to fully understand its potential and optimize its use. Several key areas warrant additional investigation to enhance the efficacy and application of PRP in wound healing.
One critical area of research is determining the optimal dosage and frequency of PRP treatment for chronic wounds. Understanding the most effective treatment protocols will help maximize the benefits of PRP and ensure consistent outcomes for patients.
Another important focus is examining the effects of PRP on wound healing in different patient populations, such as those with diabetes or vascular disease. These conditions can complicate the healing process, and tailored PRP treatments could offer significant advantages for these groups.
Comparing the efficacy of PRP to other treatments for chronic wounds, such as compression therapy or advanced wound dressings, is also crucial. This comparative research will help establish PRP’s place in the broader landscape of wound care and identify the most effective treatment combinations.
Investigating the use of PRP in combination with other therapies, such as antibiotics or additional growth factors, could further enhance wound healing. For instance, the role of vascular endothelial growth factor (VEGF) in promoting angiogenesis and tissue regeneration is a promising area of study that could complement PRP therapy.
Developing standardized protocols for the preparation and application of PRP is another essential step. Consistency in how PRP is prepared and used will help ensure reliable results and facilitate broader adoption in clinical practice.
Overall, further research is needed to fully understand the benefits and limitations of PRP treatment for chronic wounds. By exploring these areas, we can establish PRP’s place in the treatment of chronic venous leg ulcers and other chronic non-healing ulcers, ultimately improving patient outcomes and advancing the field of wound healing.
Conclusion: PRF as a Game Changer for Leg Ulcers
Venous ulcers are a challenging condition that affects millions of people worldwide. Conventional treatments often fall short of providing lasting relief, leaving patients vulnerable to complications and a reduced quality of life. However, PRF has emerged as a powerful tool in the treatment of chronic leg ulcers, offering a cost-effective, natural, and efficient solution that accelerates healing and reduces the risk of recurrence.
By leveraging the body’s own healing mechanisms, PRF provides a safe and innovative option for patients with venous ulcers, diabetic ulcers, and other chronic wounds. With its long-lasting effects, simple preparation, and high success rate, PRF can be an integral part of a comprehensive wound care strategy, helping to improve patient outcomes and quality of life.
For patients suffering from chronic or nonhealing leg ulcers, PRF represents a promising avenue for achieving faster healing and reducing the burden of the disease. Further studies with larger sample sizes and longer follow-up periods will help solidify PRF’s role as a mainstay in wound healing and regenerative medicine.